Covid-19: Family members with loved ones in nursing home endure time apart
published by Channel New Asia Digital on April 21, 2020SINGAPORE: When Mr Derrick Loke was not working, he spent time with his ailing mother – giving her massages and sharing the latest happenings in his life. Staff from the NTUC Health Nursing Home in Geylang East, where she is a resident, know him as a common fixture who visits every day without fail and stays till the end of visiting hours.
“I’ve always been close to my mum, I would discuss everything with her,” said Mr Loke.
But on the night of Apr 1, everything changed for him. He received a message from the nursing home informing him that he could not visit his mother – starting from the very next day. The Ministry of Health (MOH) and Agency for Integrated Care (AIC) had just announced that no visitors would be allowed at nursing homes in April.
This came after 10 more cases of COVID-19 at the Lee Ah Mooi Old Age Home.
“When I first heard the news, I was very lost and worried. My mum is so used to spending time with me, I’m scared she will be lonely,’ the 46-year-old said.
These days, Mr Loke checks in with his 73-year-old mother through daily 10-minute video calls, which are scheduled by the nursing home.
“I would explain to her every day that we have to do this because of the virus. I’m counting down the days with her together. I told her, we just have to endure for two more weeks, then I will come and visit you.”
Like Mr Loke, other families with loved ones in nursing homes have had to deal with the new rules even as the establishments have quickly adapted to the situation by setting up teleconferencing tools for residents.
Right after the ban on nursing home visits was announced, Mdm Rufiah Mumtaj, 60, was initially frustrated, afraid that she would not be able to see her husband for at least a month. Mr Abu Samah, 61, has been staying at the Salvation Army’s Peacehaven Nursing Home for close to three years as a stroke patient.
Normally, either her or their youngest son would be by her bed-bound husband’s side, showing him old photos of himself, massaging his legs, scratching that itch under his hand, adjusting his headphones that has P Ramlee or Elvis Presley crooning into his ears.
Their two to three hour visits have been cut short to five-, ten-minute, often one-way conversations on Skype. On these video calls, there is little she can do except to remind him why she cannot visit him right now. Sometimes, she jokingly asks if the nurses have bullied him as the caregivers snigger off-camera.
As long as she is able to see that his condition is stable, the method suffices, Mdm Rufiah said.
“I’m worried about his health,” Mdm Rufiah said about having a frail loved one amid COVID-19. “Everybody there has got low immunity. But if the circuit breaker is to protect him, then that’s good.”
Even so, she misses her husband of 32 years, particularly the tiny expressions he makes with his eyes and subtle gestures since he cannot speak.
Apparently, he is affected by their absence too, she said. In general, he has been in a good mood. But on Monday, a fever suddenly flared up, before it subsided by the next morning.
“He misses you guys,” a nurse told her.
ALLAYING RESIDENTS’ ANXIETY
The Peacehaven Nursing Home had already anticipated a need to have an alternate form of communication in the event of a pandemic and arranged for technological systems to be set up in advance, said Mr Kenny Yeo, one of its senior social workers.
They have had to explain what is happening to some puzzled residents who are used to receiving regular visits, Mr Yeo said, while to those who are cognitively impaired, the home is trying to “normalise their routine and reduce their anxiety”.
Ms Janice Tan, Head of Residential Care at NTUC Health said that family members were “very anxious” when they first heard the announcement.
“We tried our best to explain to both next-of-kin and residents on what these measures are for. For the residents, they may feel enhanced loneliness because they don’t get to see their family members.”
“But after calls have been arranged, they’ve been much more reassured and understanding of the restrictions.”
While the phone calls are typically scheduled in 10-minute time slots, Ms Tan said NTUC Health nursing homes are not strict on extensions and they will “try to accommodate as much as possible”.
“Scheduling daily video calls helps to keep residents connected with familiar faces, so they can feel comforted, reassured and know that their families are safe and sound.”
Technology may have given family members a peace of mind, but Mr Loke said it will never be the same.
“I miss her a lot, a lot. Every time I see her face through the video call, I feel very sad because I can’t go near her. Sometimes she will be sleepy and won’t respond but I’ll just continue talking to her. I know she is listening to me.”
STRAIN ON HOSPICES
While visits are still allowed at hospices, precautionary measures have had to be put in place, such as a reduction in the number of guests and shorter visitation hours.
At Assisi Hospice, where inpatients are mostly critically ill with a prognosis of 3 months, there were no visitation restrictions before COVID-19. Ever since the start of the “circuit-breaker” period, every patient is allowed four designated visitors but at any one time, only two people can visit.
“It is a bit of a challenge for end-of-life patients. When patients are dangerously ill and are expected to pass away within the next few days, it’s natural that families would want to spend more time but (some) are unable to,” said Assisi Hospice’s spokesperson.
Especially for larger families, it can be “very tough” to appoint four members as designated visitors.
“I’ve seen grandchildren who cannot visit their grandfather. It’s very, very sad. They will find all kinds of reasons but they also know it’s a restriction.”
Mdm Sa’ani Jamari has been battling stage 4 lung cancer and was given a prognosis of “a few weeks” as of Apr 13. Deciding who should visit the 70-year-old has been a challenge, given that she has five siblings, said grand-niece Sorfina Batrisyia Abdul Rahman.
“We had to choose it according to who is likely to visit more often. Not being able to include everyone’s names made some of them upset and it affected them a lot.”

Ms Sorfina Batrisyia is a designated visitor, along with her parents and cousin. Mdm Sa’ani asked “a lot of times” if she could see her other family members but video contact is the best she can get for now.
Dover Park Hospice has cut its visiting hours from 7am to
10pm, to 11am to 7pm as to limit movements within the hospice and minimise patients’ potential exposure to the coronavirus, said its chief executive, Mr Timothy Liu.
Each patient can only see two visitors on their designated list at any one time, unlike old times when there were no curbs on the number of visitors. Instead, the hospice encourages patients to have video calls.
“It is difficult to tell family members that they are not allowed to visit their loved ones who are critically ill (so) we control the numbers sensitively and still allow family members to continue to visit and spend some time with their loved ones based on compassionate grounds,” Mr Liu said.
The restrictions on movements have caused a stretch on manpower, an HCA Hospice Care spokesperson said. The agency provides home and day hospice care – it does not run an in-patient facility – to almost 1,000 people.
Now that volunteer befrienders have had to stop visits to clients who live alone, social workers have to make more rounds and calls to monitor these isolated patients. And since many patients’ hospital appointments have been postponed, the clinical team makes more frequent check-ins on patients with ‘active dying’ symptoms.
PROVIDING A SENSE OF NORMALCY
With the ban on nursing home visits, volunteer activities have had to be stopped as well. In the past, volunteers would visit NTUC Health’s nursing homes to befriend seniors, play games or teach art and craft.
“We’ve started to make modifications on activities that we used to do, while making sure distances are kept,” said Ms Tan. For example, exercises and games are now conducted via tutorials on televisions or tablets.
“Our staff working from home also got creative and started doing live cooking shows which the residents can watch. They can interact and respond to one another, which keeps the interaction alive.”
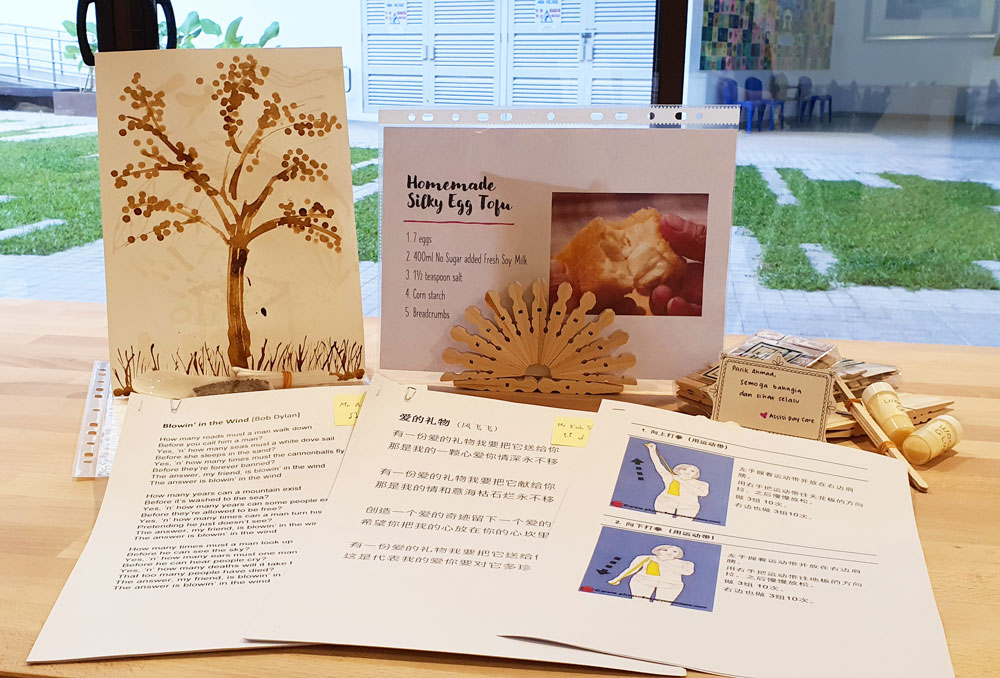
Assisi Hospice is putting together a penpal programme with volunteers, since they are unable to visit the inpatients. On some days, staff are also delivering special hawker meals donated by volunteers.
As for daycare patients who have to stay home now, Assisi Hospice are sending them “home-based learning” packs based on their interest groups.
“For example, our occupational therapist has prepared a recipe in a language that they are familiar with for those in the cooking interest group. We will provide video instructions and our team will also call to check on them,” its spokesperson said.
Keeping them engaged and occupied is important for their psycho-social well being, so they don’t feel lonely or isolated, added Ms Tan.
“Continuing with activities like exercises and games on a daily basis, though remotely, gives them a sense of normalcy. We make the best in the worst of times.”
Click Here to view full article

